What Is Treatment-Emergent Central Sleep Apnea?
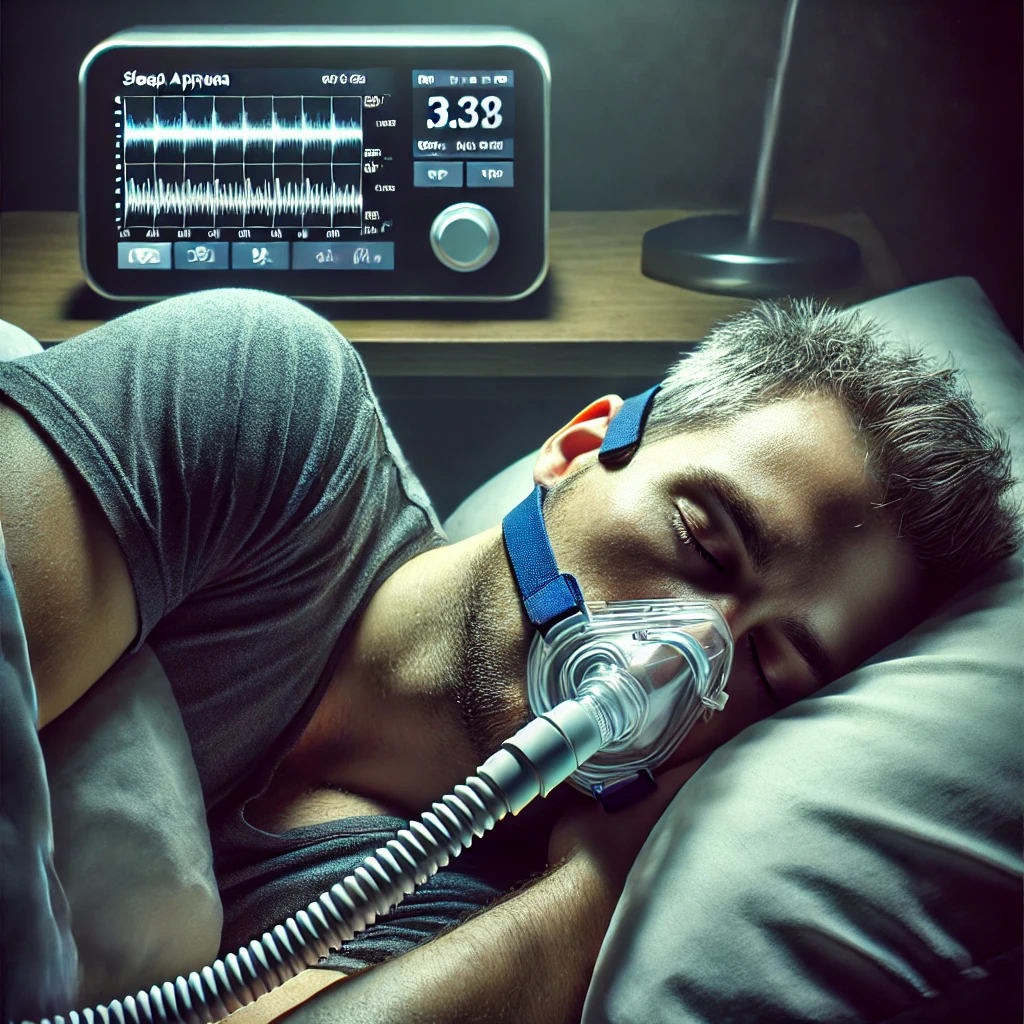
Treatment-emergent central sleep apnea (TECSA) occurs when central sleep apnea (CSA) develops after starting CPAP or BiPAP therapy for obstructive sleep apnea (OSA). Instead of improving breathing, CPAP therapy sometimes disrupts the brain’s ability to regulate breathing, causing pauses during sleep.
This condition affects 5-15% of CPAP users, though many cases resolve naturally over time. However, for individuals experiencing persistent TECSA, further evaluation and specialized treatment may be necessary.
Causes of Treatment-Emergent Central Sleep Apnea
Several factors contribute to the development of TECSA. The most common causes include:
✔ High CPAP pressure – Excessive air pressure may lead to over-ventilation, reducing carbon dioxide (CO₂) levels and causing breathing instability.
✔ Pre-existing breathing control issues – Some individuals have an underlying CO₂ regulation sensitivity, making them prone to central sleep apnea.
✔ Heart failure or neurological conditions – Certain conditions, such as congestive heart failure or brainstem disorders, can worsen apnea symptoms.
✔ Altitude changes – Higher elevations impact breathing regulation, increasing the likelihood of central apnea episodes.
Symptoms of Treatment-Emergent Central Sleep Apnea
Recognizing TECSA can be difficult since its symptoms often overlap with obstructive and central sleep apnea. Some of the most common signs include:
✔ Pauses in breathing lasting 10 seconds or more
✔ Excessive daytime fatigue and drowsiness
✔ Gasping or choking sensations upon waking
✔ Difficulty falling or staying asleep (insomnia-like symptoms)
✔ Morning headaches and brain fog
✔ Poor CPAP tolerance or worsening sleep quality after using CPAP
How TECSA Is Diagnosed
A follow-up sleep study (polysomnography) is required to determine if CPAP therapy is triggering treatment-emergent central sleep apnea. The study monitors breathing patterns, oxygen levels, and apnea events, allowing sleep specialists to assess whether central apnea episodes have increased since initiating CPAP treatment.
Treatment Options for TECSA
1. Monitor Symptoms & Continue CPAP Therapy
Many cases of TECSA resolve on their own within 2-3 months. Sleep specialists often recommend continuing CPAP therapy while tracking symptoms to see if they gradually improve.
2. Adjust CPAP Pressure Settings
High CPAP pressure can trigger central apneas by lowering CO₂ levels excessively. Making adjustments, such as reducing pressure or enabling adaptive pressure settings, can help stabilize breathing patterns.
3. Switch to BiPAP or Adaptive Servo-Ventilation (ASV)
For persistent cases, switching to a BiPAP (bilevel positive airway pressure) or ASV device may provide relief. Unlike CPAP, ASV technology automatically adapts pressure levels to support stable breathing.
4. Address Underlying Health Conditions
Managing heart disease, neurological disorders, or medication-induced apnea is essential in cases where an underlying condition is contributing to TECSA. Treating these conditions may significantly reduce apnea episodes.
5. Oxygen Therapy & CO₂ Rebreathing Techniques
Some individuals require supplemental oxygen or CO₂ rebreathing therapy to stabilize breathing and prevent frequent apnea episodes. A sleep specialist can determine if this approach is suitable.
Final Thoughts
Treatment-emergent central sleep apnea can be a frustrating condition, especially when it develops after starting CPAP therapy. While many cases resolve naturally, some require adjustments to CPAP settings, alternative therapies, or medical intervention. If you’ve noticed worsening sleep quality or unusual breathing patterns since beginning CPAP, consulting a sleep specialist can help determine the best course of action.